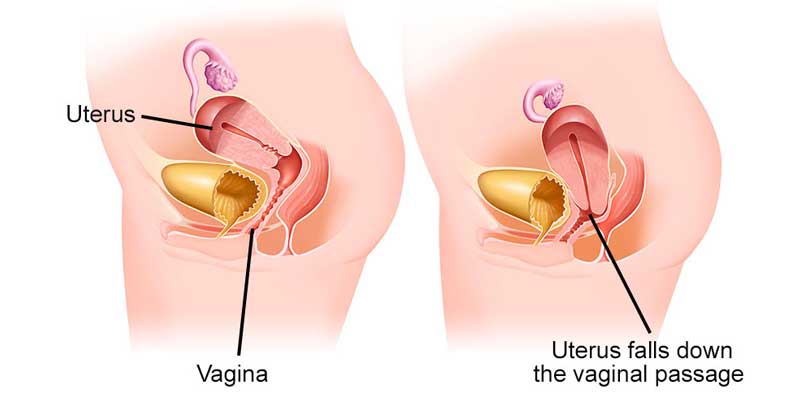
Uterine prolapse is a condition where the muscles and tissues around your uterus become weak. This causes your uterus to sag or drop down into your vagina. It can happen to anyone assigned female at birth (AFAB), but is most common after menopause and in people who’ve had more than one vaginal delivery.
The muscles, ligaments and tissues in your pelvis are called your pelvic floor muscles. These muscles support your uterus, rectum, vagina, bladder and other pelvic organs. A prolapse occurs when your pelvic floor muscles are damaged or weakened to the point where they can no longer provide support. This causes your pelvic organs to drop into or out of your vagina.
Uterine prolapse can be mild or severe depending on how weak the supporting muscles of your uterus have become. In an incomplete prolapse, your uterus may have slipped enough to be partway in your vagina. This creates a lump or bulge. In a more severe case, your uterus can slip far enough that it comes out of your vagina. This is called a complete prolapse.
1.Vaginal Repair:This minimally invasive procedure involves accessing the prolapsed uterus through the vagina. The weakened pelvic floor tissues are repaired and reinforced, often using stitches or surgical mesh to provide additional support. The uterus is then repositioned, and the vaginal wall is closed.
2.Abdominal Repair:In some cases, an abdominal approach may be necessary. This involves making an incision in the abdomen to access and repair the prolapsed uterus. This approach is often used when other pelvic organs are also prolapsed.
3.Laparoscopic Repair:This minimally invasive procedure uses small incisions and a laparoscope (a thin, lighted tube) to view and repair the prolapsed uterus. The laparoscopic approach offers a quicker recovery time and less post-operative pain compared to traditional open surgery.
Alleviates symptoms such as pelvic pressure, discomfort, and urinary incontinence.
Restores normal function of the pelvic organs and improves quality of life.
Minimally invasive options available with quicker recovery times.
After the surgery, Dr. Manchanda and her team will provide detailed post-operative care instructions, including pain management, activity restrictions, and guidance on pelvic floor exercises to strengthen the supporting muscles. Patients will be monitored for any signs of complications and will have follow-up appointments to ensure proper healing and the success of the repair.
2024 Dr. Prabhjot Manchanda Designed and Developed by EDM